Sunday, 7 December 2014
Clostridium perfringens
Sunday, 7 December 2014 by Unknown
Clostridium perfringens

C. perfringens
Clostridium perfringens, which produces a huge array of invasins and exotoxins, causes wound and surgical infections that lead to gas gangrene, in addition to severe uterine infections. Clostridial hemolysins and extracellular enzymes such as proteases, lipases, collagenase and hyaluronidase, contribute to the invasive process. Clostridium perfringens also produces an enterotoxin and is an important cause of food poisoning. Usually the organism is encountered in improperly sterilized (canned) foods in which endospores have germinated.
Food poisoning
Gas gangrene
Gas gangrene generally occurs at the site of trauma or a recent surgical wound. The onset of gas gangrene is sudden and dramatic. About a third of cases occur on their own. Patients who develop this disease in this manner often have underlying blood vessel disease (atherosclerosis or hardening of the arteries), diabetes, or colon cancer.
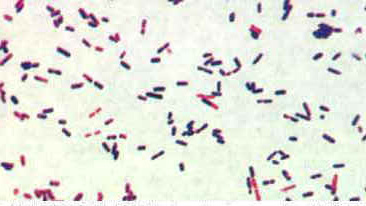
Clostridium perfringens, Gram Stain. Most clostridia are renowned for staining "Gram-variable".
Tags:
BACTERIAL PATHOGEN ,
INSTANT NOTES ,
PATHOGEN

C. perfringens
Clostridium perfringens, which produces a huge array of invasins and exotoxins, causes wound and surgical infections that lead to gas gangrene, in addition to severe uterine infections. Clostridial hemolysins and extracellular enzymes such as proteases, lipases, collagenase and hyaluronidase, contribute to the invasive process. Clostridium perfringens also produces an enterotoxin and is an important cause of food poisoning. Usually the organism is encountered in improperly sterilized (canned) foods in which endospores have germinated.
Food poisoning
Clostridium perfringens is classified into 5 types (A�E) on the basis of its ability to produce one or more of the major lethal toxins, alpha, beta, epsilon and iota (α, β, ε, and ι). Enterotoxin (CPE)-producing (cpe+) C. perfringens type A is reported continuously as one of the most common food poisoning agents worldwide. An increasing number of reports also implicate the organism in 5%�15% of antibiotic�associated diarrhea (AAD) and sporadic diarrhea (SD) cases in humans, as well as diarrhea cases in animals.
Most food poisoning strains studied carry cpe in their chromosomes; isolates from AAD and SD cases bear cpe in a plasmid. Why C. perfringens strains withcpe located on chromosomes or plasmids cause different diseases has not been satisfactorily explained. However, the relatively greater heat resistance of the strains with chromosomally located cpe is a plausible explanation for these strains' survival in cooked food, thus causing instances of food poisonings. The presence of C. perfringens strains with chromosomally located cpe in 1.4% of American retail food indicates that these strains have an access to the food chain, although sources and routes of contamination are unclear.
An explanation for the strong association between C. perfringens strains with plasmid-located cpe and cases of AAD and SD disease may be in vivo transfer of the cpe plasmid to C. perfringens strains of the normal intestinal microbiota. Thus, a small amount of ingested cpe+ C. perfringens would act as an infectious agent and transfer the cpe plasmid to cpe� C. perfringens strains of the normal microbiota. Conjugative transfer of the cpe plasmid has been demonstrated in vitro, but no data exist on horizontal gene transfer of cpe in vivo, and whether cpe+ strains that cause AAD and SD are resident in the gastrointestinal tract or acquired before onset of the disease is unknown.
Case Study
Report of C. perfringens Food Poisoning
Report of C. perfringens Food Poisoning
Clostridium perfringens is a common cause of outbreaks of foodborne illness in the United States, especially outbreaks in which cooked beef is the implicated source. This is a condensed version of an MMWR report that describes an outbreak of C. perfringens gastroenteritis following St. Patrick's Day meals of corned beef. The report typifies outbreaks of C. perfringens food poisoning.
Report
On March 18, 1993, the Cleveland City Health Department received telephone calls from 15 persons who became ill after eating corned beef purchased from one delicatessen. After a local newspaper article publicized this problem, 156 persons contacted the health department to report onset of diarrheal illness within 48 hours of eating food from the delicatessen on March 16 or March 17. Symptoms included abdominal cramps (88%) and vomiting (13%); no persons were hospitalized. The median incubation period was 12 hours (range: 2-48 hours). Of the 156 persons reporting illness, 144 (92%) reported having eaten corned beef; 20 (13%), pickles; 12 (8%), potato salad; and 11 (7%), roast beef.
On March 18, 1993, the Cleveland City Health Department received telephone calls from 15 persons who became ill after eating corned beef purchased from one delicatessen. After a local newspaper article publicized this problem, 156 persons contacted the health department to report onset of diarrheal illness within 48 hours of eating food from the delicatessen on March 16 or March 17. Symptoms included abdominal cramps (88%) and vomiting (13%); no persons were hospitalized. The median incubation period was 12 hours (range: 2-48 hours). Of the 156 persons reporting illness, 144 (92%) reported having eaten corned beef; 20 (13%), pickles; 12 (8%), potato salad; and 11 (7%), roast beef.
In anticipation of a large demand for corned beef on St. Patrick's Day (March 17), the delicatessen had purchased 1400 pounds of raw, salt-cured product. Beginning March 12, portions of the corned beef were boiled for 3 hours at the delicatessen, allowed to cool at room temperature, and refrigerated. On March 16 and 17, the portions were removed from the refrigerator, held in a warmer at 120oF (48.8oC), and sliced and served. Corned beef sandwiches also were made for catering to several groups on March 17; these sandwiches were held at room temperature from 11 a.m. until they were eaten throughout the afternoon.
Cultures of two of three samples of leftover corned beef obtained from the delicatessen yielded greater than or equal to 105 colonies of C. perfringens per gram.
Following the outbreak, public health officials recommended to the delicatessen that meat not served immediately after cooking be divided into small pieces, placed in shallow pans and chilled rapidly on ice before refrigerating, and that cooked meat be reheated immediately before serving to an internal temperature of greater than or equal to 165oF (74 C).
Analysis
C. perfringens is a ubiquitous, anaerobic, Gram-positive, spore-forming bacillus and a frequent contaminant of meat and poultry. C. perfringens food poisoning is characterized by onset of abdominal cramps and diarrhea 8-16 hours after eating contaminated meat or poultry. By sporulating, this organism can survive high temperatures during initial cooking; the spores germinate during cooling of the food, and vegetative forms of the organism multiply if the food is subsequently held at temperatures of 60-125oF (16-52oC). If served without adequate reheating, live vegetative forms of C. perfringens may be ingested. The bacteria then elaborate the enterotoxin that causes the characteristic symptoms of diarrhea and abdominal cramping.
C. perfringens is a ubiquitous, anaerobic, Gram-positive, spore-forming bacillus and a frequent contaminant of meat and poultry. C. perfringens food poisoning is characterized by onset of abdominal cramps and diarrhea 8-16 hours after eating contaminated meat or poultry. By sporulating, this organism can survive high temperatures during initial cooking; the spores germinate during cooling of the food, and vegetative forms of the organism multiply if the food is subsequently held at temperatures of 60-125oF (16-52oC). If served without adequate reheating, live vegetative forms of C. perfringens may be ingested. The bacteria then elaborate the enterotoxin that causes the characteristic symptoms of diarrhea and abdominal cramping.
Laboratory confirmation of C. perfringens foodborne outbreaks requires quantitative cultures of implicated food or stool from ill persons. This outbreak was confirmed by the recovery of greater than or equal to 105 organisms per gram of epidemiologically implicated food. An alternate criterion is that cultures of stool samples from persons affected yield greater than or equal to 106 colonies per gram. Stool cultures were not done in this outbreak. Serotyping is not useful for confirming C. perfringens outbreaks and, in general, is not available.
Corned beef is a popular ethnic dish that is commonly served to celebrate St. Patrick's Day. The errors in preparation of the corned beef in this outbreak were typical of those associated with previously reported foodborne outbreaks of C. perfringens. Improper holding temperatures are a contributing factor in most C. perfringens outbreaks reported to CDC. To avoid illness caused by this organism, food should be eaten while still hot or reheated to an internal temperature of greater than or equal to 165oF (74oC) before serving.Gas gangrene
Gas gangrene generally occurs at the site of trauma or a recent surgical wound. The onset of gas gangrene is sudden and dramatic. About a third of cases occur on their own. Patients who develop this disease in this manner often have underlying blood vessel disease (atherosclerosis or hardening of the arteries), diabetes, or colon cancer.
Clostridium perfringens produces many different toxins, four of which (alpha, beta, epsilon, iota) can cause potentially deadly syndromes. The toxins cause damage to tissues, blood cells, and blood vessels.
Gas gangrene is marked by a high fever, brownish pus, gas bubbles under the skin, skin discoloration, and a foul odor. It is the rarest form of gangrene, and only 1,000 to 3,000 cases occur in the United States each year. It can be fatal if not treated immediately.
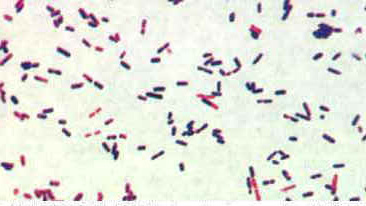
Clostridium perfringens, Gram Stain. Most clostridia are renowned for staining "Gram-variable".
Subscribe to:
Post Comments (Atom)


0 Responses to “Clostridium perfringens ”
Post a Comment